
Key Questions to Ask in a Classroom on Managing Lower Respiratory Disorders in Children
Teaching the management of lower respiratory disorders in children requires navigating a broad range of symptoms, treatments, and underlying conditions. To help students fully understand this vital aspect of pediatric care, it is important to use thought-provoking questions that encourage critical thinking and deepen their comprehension. Here is a guide to essential questions that should be discussed in a classroom setting focused on managing lower respiratory disorders in children.
1. What Are the Common Lower Respiratory Disorders in Children?
Why It Matters: Understanding the range of disorders is foundational to effective management and treatment.
Examples of Questions: What are the most prevalent lower respiratory disorders seen in pediatric patients?
How do conditions like asthma, bronchiolitis, and pneumonia differ in their presentation and management?
2. How Do You Differentiate Between Viral and Bacterial Lower Respiratory Infections?
Why It Matters: Accurate diagnosis is crucial for determining the appropriate treatment approach.
Examples of Questions: What clinical signs and symptoms help differentiate between viral and bacterial lower respiratory infections in children?
What diagnostic tests are useful in distinguishing between these types of infections?
3. What Are the Key Components of a Comprehensive Assessment for Lower Respiratory Disorders?
Why It Matters: A thorough assessment is critical for developing an effective treatment plan.
Examples of Questions: What history and physical examination findings are essential when assessing a child with suspected lower respiratory disorders?
How should clinicians use imaging and laboratory tests in the assessment process?
4. How Do You Develop an Effective Management Plan for Each Disorder?
Why It Matters: Tailoring management plans to specific conditions ensures targeted and effective treatment.
Examples of Questions: What are the main treatment strategies for managing asthma in children, and how do they vary with severity?
How should treatment for bronchiolitis differ from that for pneumonia?
5. What Are the Key Pharmacological and Non-Pharmacological Treatments?
Why It Matters: Understanding various treatment options helps in crafting comprehensive management plans.
Examples of Questions: What are the first-line pharmacological treatments for common lower respiratory disorders in children?
What non-pharmacological interventions can support respiratory health and improve outcomes?
6. How Do You Monitor and Evaluate Treatment Effectiveness?
Why It Matters: Ongoing evaluation ensures that treatment plans are effective and adaptable to the child’s needs.
Examples of Questions: What indicators should clinicians monitor to assess the effectiveness of treatment for lower respiratory disorders?
How can clinicians adjust treatment plans based on the child's response and progress?
7. What Are the Potential Complications and How Can They Be Managed?
Why It Matters: Awareness of potential complications helps in preventing and addressing adverse outcomes.
Examples of Questions: What complications are associated with untreated or poorly managed lower respiratory disorders in children?
How can clinicians prevent or address these complications?
8. How Do You Educate Families and Caregivers About Managing Lower Respiratory Disorders?
Why It Matters: Effective education empowers families to support their child's care and recognize symptoms.
Examples of Questions: What key information should be provided to families and caregivers about managing their child’s lower respiratory disorder?
How can healthcare providers effectively communicate with families to ensure they understand the management plan and follow-up needs?
9. What Role Does Follow-Up Care Play in Managing Lower Respiratory Disorders?
Why It Matters: Regular follow-up ensures continuity of care and early intervention if issues arise.
Examples of Questions: How often should children with lower respiratory disorders be seen for follow-up visits?
What aspects of care should be addressed during follow-up appointments?
10. How Do You Address the Special Needs of Children with Chronic Lower Respiratory Conditions?
Why It Matters: Chronic conditions require ongoing management and tailored care strategies.
Examples of Questions: What are the unique challenges in managing chronic lower respiratory disorders in children?
How can care be adjusted to meet the long-term needs of children with chronic respiratory conditions?
Addressing these key questions in a classroom focused on managing lower respiratory disorders in children can significantly enhance students' understanding and preparedness. By exploring these areas, educators can ensure that future healthcare professionals are well-equipped to diagnose, treat, and manage lower respiratory conditions effectively, ultimately improving patient outcomes and advancing pediatric care.
According to Primary Care Pediatrics for the Nurse Practitioner, Infants have increased chest wall compliance. Chest wall compliance becomes more pronounced during periods of respiratory distress when intercostal retractions are present. Practitioners should be alert for common signs of respiratory distress in children, such as increased respiratory rate, retractions, grunting, cyanosis, abnormal body positions at rest, use of accessory muscles, and the presence of adventitious breath sounds (University of Rochester Medical Center, 2020).
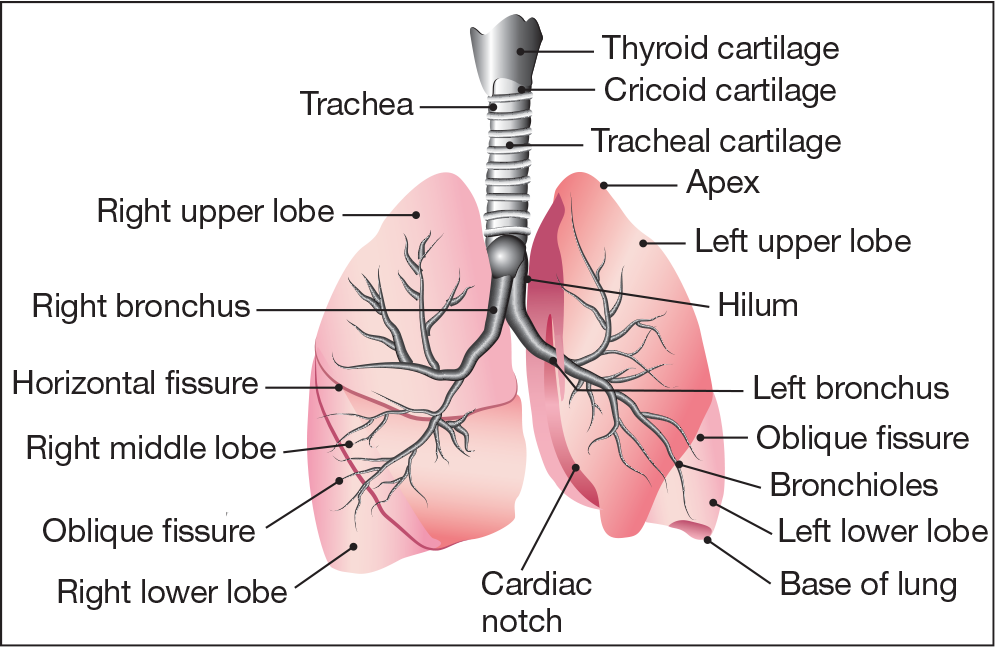
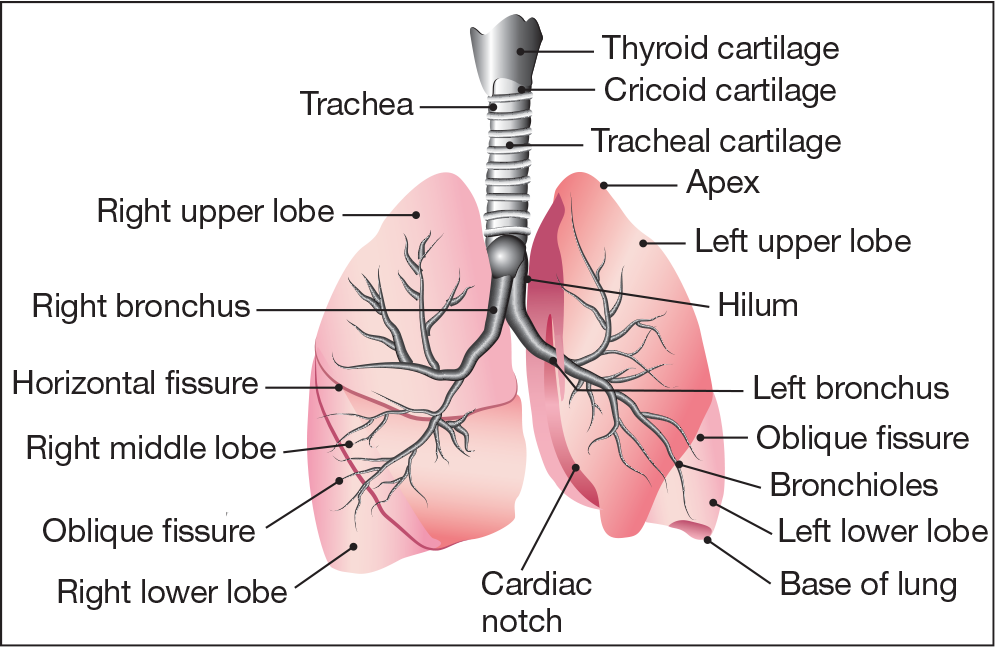
Lower respiratory issues in children, including viral and bacterial infections (such as bronchiolitis and pneumonia) and chronic conditions (like asthma), are frequently encountered. Accurate diagnosis requires a comprehensive health history, a detailed physical examination of the respiratory system, and, if needed, the ordering and interpretation of laboratory and diagnostic tests. It is crucial to teach your students how to make precise diagnoses, as this is fundamental for creating effective treatment and management plans. Additionally, helping your students understand that a thorough and systematic assessment of respiratory status is essential for identifying potentially life-threatening conditions is vital.
Prepare your student nurses to provide outstanding care to children of all ages with our broad selection of resources tailored for success in pediatric nursing.
Select the titles that interest you and request an exam copy for review today!



